1. Introduction to Rehabilitation and Surgeries
Rehabilitation and surgeries represent two interconnected aspects of modern healthcare. While surgery is often necessary to treat acute medical conditions, injuries, or chronic issues, rehabilitation ensures that patients regain strength, mobility, and independence post-surgery. Together, these disciplines form the foundation for a holistic approach to healing.
The process begins with identifying the patient's medical needs, which could range from orthopedic surgeries for fractures to complex cardiac procedures. Regardless of the type, rehabilitation plays a crucial role in restoring quality of life. This section delves into the growing significance of these interrelated fields and their profound impact on patient outcomes.
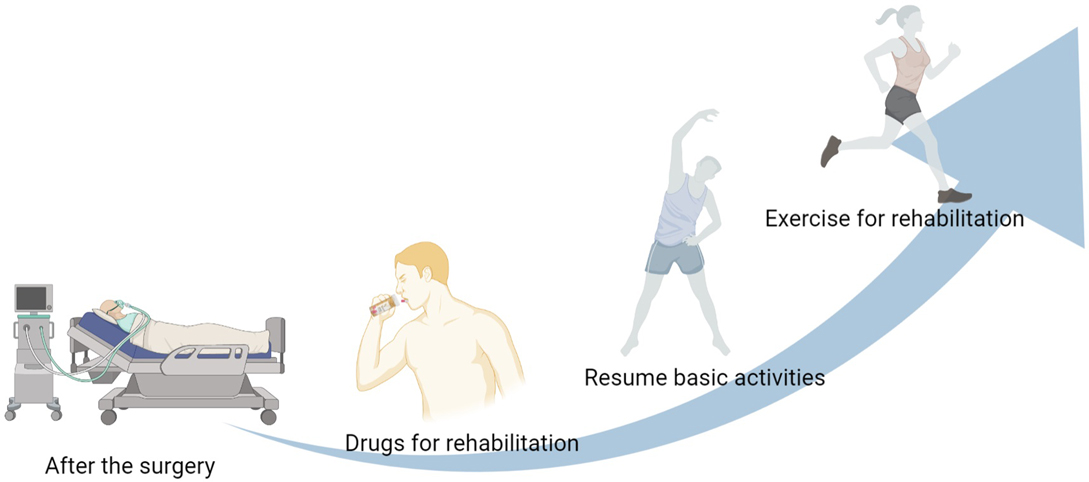
2. The Role of Rehabilitation in Postoperative Recovery
Postoperative rehabilitation is essential for helping patients transition from surgery to everyday life. It minimizes complications such as infections, blood clots, or joint stiffness. A comprehensive rehabilitation program includes physical therapy, occupational therapy, and psychological support.
Physical therapy focuses on restoring mobility and strength through exercises and techniques that reduce pain and swelling. Occupational therapy helps patients relearn daily tasks and adapt to new physical limitations. Furthermore, addressing the mental health aspect through counseling and support groups ensures emotional resilience during recovery.

3. Types of Surgeries and Their Impacts
Surgeries can be broadly categorized into elective, emergency, minimally invasive, and open procedures. Each type comes with unique challenges and recovery timelines.
- Elective surgeries include planned procedures like joint replacements or cosmetic surgeries.
- Emergency surgeries are life-saving interventions, such as appendectomies or trauma surgeries.
- Minimally invasive surgeries (e.g., laparoscopic procedures) have revolutionized healthcare with shorter recovery periods and reduced risks.
- Open surgeries, while more invasive, remain essential for complex conditions like organ transplants.
Understanding the implications of each surgery type helps healthcare providers tailor rehabilitation plans to suit individual needs.
:max_bytes(150000):strip_icc()/Untitleddesign78-da6e618aecd44b86a0c487caec0a2243.jpg)
4. Designing Personalized Rehabilitation Plans
Personalized rehabilitation plans are at the heart of effective recovery. These plans consider factors such as the patient’s age, medical history, and the nature of the surgery.
- Assessment Phase: A thorough evaluation by healthcare professionals determines the patient’s physical and psychological condition.
- Goal Setting: Clear, achievable milestones are established to guide the recovery process.
- Implementation: Rehabilitation exercises, dietary plans, and therapies are administered in stages to prevent overexertion.
Patient involvement and consistent monitoring ensure that the plan adapts to progress or setbacks, resulting in a smoother recovery journey.

5. Innovations in Surgery and Rehabilitation
Advancements in medical technology have transformed both surgery and rehabilitation. Robotic surgeries, 3D printing for prosthetics, and AI-driven diagnostics enhance surgical precision and outcomes.
In rehabilitation, innovations like virtual reality (VR) for physical therapy, wearable technology for progress tracking, and telerehabilitation services expand access to care. These tools empower patients to engage in their recovery actively and efficiently.
6. The Future of Integrated Care
The integration of surgery and rehabilitation into seamless care pathways represents the future of healthcare. Multidisciplinary teams, including surgeons, therapists, and nutritionists, collaborate to create comprehensive treatment plans.
Emerging trends such as precision medicine and regenerative therapies promise to further personalize and enhance patient care. As healthcare continues to evolve, the synergy between surgeries and rehabilitation will remain pivotal in improving patient outcomes and quality of life.


You must be logged in to post a comment.