In modern medicine, surgical site infections are still a significant issue. Staphylococcus epidermidis present on the skin and circulating or scrubbed personnel cause most of the infection while following the sterile surgery.
The infection at the surgical site or the vicinity of the surgical site incision contributed greatly to causing disease and deaths within 20-30 days every year. Surgical site infections cause 13-16% of hospital-acquired infections and diseases. Among hospitalized patients, it represents the most frequent hospital-acquired infection. Advanced technologies used for infection control include filtered ventilation (Laminar-air flow with HEPA filters) in the operation theatre, sterilization methods, surgical techniques, and the prevention of infection by antimicrobial therapy. Regardless of these preventive measures, surgical site infections are still a significant cause of diseases and deaths among patients admitted to hospitals. Airborne contamination greatly involves surgical site infection that should be prevented by the latest technology such as laminar air-flow with HEPA filters.
To minimize morbidity rates and expenses associated with hospital-acquired infections, the sources of pathogen transmission must be reduced. To achieve the goal of reducing pathogen transmission in hospitals, a particular dress for staff such as nurses, surgeons, technicians, and sweepers working in operation theatres should be assigned. The other factors involved in reducing pathogen transmission are patient preparation (patient gowning and draping), operation theatre design, and the use of air filters for controlled ventilation. We should consider the source of pathogen transmission while investing in measures that reduce and control pathogen transmission efficiently and reduce the patient’s stay in the hospital.
Experimental analysis of factors causing airborne particle dispersion in operation theatre
Between 1986 and 1996, the National Nosocomial Infection System reported more than 15000 surgical site infections from more than 590000 operations, and about 77% mortality was reported resulting from the surgical site infections
“One of the major sources of exogenic bacteria that cause contamination is airborne particles”
We have experimental analysis and its results to observe the flow and number of particles originating from the activities performed in the operation theatre by staff nurses.
All surgical garments used in the experiment were made from 45% wood pulp while 55% polyester pulp, a non-woven fabric. The surgical drapes and the other garments should be soaked with a “fluid-repellent” and made lint-free. The surgical garments had defined conditions i.e. resistance to bacterial penetration, lint-free, stretchable, etc should be concerned with manufacturers and distributors
Instrument table preparation
To drape the instrument table, the scrubbed nurse unfolded a sterile drape and covered the instrument table which spread particles in an anteroinferior direction detected by a fine visualization system. Most of the particles were sized 0.3 to 0.5 microns.
Donning/doffing gloves and gowns
The particle dispersion while unfolding a surgical sterile gown (Fig. A), is similar to the unfolding of the surgical sterile drapes i.e. anteroinferior direction.
Furthermore, a lot of particles were spread while removing gloves, these particles were considered to be sweat, the latex of gloves, and skin tissues
performed in an ultra-clean zone with a downward air curtain, while about 75% when the surgical staff wore sterile personal protective equipment Microbiological sanitation standards already exist for the air in which products with sterile solutions and drug infusions or other goods that contact with body fluids or the wounds
Improved ventilation using HEPA filter with the laminar air-flow system
The latest operation theatres have formal plenum ventilation, by using filters with up to 95% efficiency to block the particles present in the air, less than or equal to 5micron (Standard, 1956). HEPA filters in combination with a laminar airflow system remove air particles of 0.3mm and with 99.97% efficacy for the surgeries that use implants. The HEPA filter with the laminar airflow mechanism could be installed in the operating rooms by either the ceiling-mounted or wall-mounted, vertical flow, and horizontal flow units respectively
The vertical and horizontal laminar air-flow system
The airflow is separated into small linear columns of cold air, which generate a low velocity and blow it towards the sterile area. Objects that produce heat clouds, such as light bulbs, team members, or equipment can change the airflow in, different directions
Vertical airflow has fewer hindrances to the line of direction of the airflow. Vertically downward flow of air is intended to flow from the ceiling of the room, over the lights, patients, and equipment, and continue downward creating a canopy toward the inferior corners of the room where they meet the air return grills. When vertical laminar airflow is used aptly, it shows an 86-89% reduction in colony-forming units
In current operating rooms, there are three designs of vertical downward directed airflow arising from the top of the room/ceiling directly bunched over the field with little difference in effects
a. At the Mayo Clinic USA, the horizontal airflow (figure 1.1), the clean zone system was used in which a whole wall was utilized as a source of “microbiologically” clean air. Even though these arrangements were highly expensive.
b. The horizontal airflow goes through the wall outlet to an opposite lower return air vent. Objects in the path of the airflow throw particles into the filtered airstream (Phillips, 2016). Standard vertical laminar airflow presents a narrow perimeter of the working area that starts on the ceiling and interacts with the field, staff, and ambient room air earlier than it is exhausted via air return vents without air curtains.
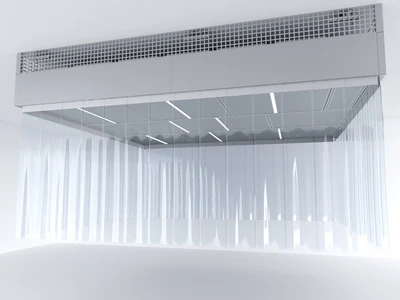
c. Vertical flow with air curtains uses higher velocity peripheral, secondary airflow to expand and frame the primary laminar flow from the ceiling to the lower pressure return air vents at the base of the walls.
d. Physical curtains that hang from the ceiling use air sheets on four sides to maintain the downward direction of the air stream. In this way, the air is directed onto the field and flows around and behind the surgical team which produces a heat plume that changes the direction of the airflow.
To resolve the inconveniences related to vertical airflow, a horizontal laminar airflow system was established, but this system also has some major problems, the unidirectional airflow disrupted by the members of an operating room. “Although few studies have shown that the vertical laminar airflow produces lesser microbes at the surgical site”
In the late 2000s, portable UV systems were used routinely in operating theatres nightly, and in some situations, between cases, these mobile devices eliminated the need for heavy protective equipment and the operator removed them from the room before human exposure. Table 2.1 shows some advantages and disadvantages of portable versus fixed UVC disinfection devices.
Pros and Cons of portable versus fixed UVC disinfection devices
“Despite longer cycles in fixed UVC devices, housekeepers are free to continue other activities like manual cleaning of other operating rooms while UV disinfection is taking place. A tablet tracks the progress of disinfection taking place”.
Multi-position portable UVC light required only two 5-min cycles on each side of the operating table to fully disinfect the high-touch surfaces in the room

Conclusion
In the history of performing surgeries, surgical site infection has been a complex problem for a long time. It is more difficult to deal with the problems that arise after surgery. Many technologies have been used to solve these problems such as HEPA filters, the laminar airflow system, and the Ultraviolet light treatment or ultraviolet germicidal irradiation. The infection rate reduced to a great extent in operation theaters where these applications have been used. The role of these applications is to block the entrance of microbes and other dust particles along with the air in the operation theater preventing surgical site infection by providing filtered air in an operating room. Ultraviolet germicidal irradiations kill the pathogen present in an operating room environment and prevent wound infection after surgery. The surgical site infection will cause a burden on the patient by increasing their expenses due to long time stay in hospital and it also increases the stress on the patient and their attendants. The advancement in technology regarding the clean environment is still going on which will be very beneficial for the patient.

You must be logged in to post a comment.